Anthropologist Testifies Before California Task Force on Reparations
IPR anthropologist Christopher Kuzawa emphasizes that reparations must consider physical health inequities
Get all our news
This is partly a story about how health inequality today traces to racial injustices in the past, but it also shows that policy changes that improve things now are going to have benefits that reverberate into the future as well. ”
Christopher Kuzawa
IPR anthropologist
In 2020, California established a Reparations Task Force to study “the institution of slavery and its lingering negative effects on living African Americans” and develop proposals for reparations. It released its landmark report and recommendations on June 29.
In testifying before it last year, IPR biological anthropologist Christopher Kuzawa spoke about his and others’ work that uncovers the drivers behind U.S. social inequities and emphasized the importance of inequities in physical health when considering the issue of reparations.
He outlined stark differences in life expectancy: Black women live three years less and Black men live four and a half years less than Whites on average. He attributes these differences to long-term chronic conditions, like diabetes and high-blood pressure. In underscoring that genes are important but “not a cause,” he explained the evidence for understanding race as a social construct—“not based on something genetic and objective.” Rather, “chronic differences” in social factors like education, stress, and economic opportunity are major drivers of these stark health and biological differences.
Kuzawa then explained his findings from a decades-long, multigenerational study in the Philippines. They indicate how life experiences from in utero and infancy can influence a person’s health and life chances as an adult: Babies with low birth weights who became overweight as adults faced a 25% increase in getting a chronic disease.
“The idea here is that the roots of adult health trace in part to intrauterine and early postnatal life,” he told the task force, “and this is an important part of the overall story of the social origins of health and inequality in this country.”
Epigenetics, which he describes as a “biological memory” of chemical changes to people’s chromosomes, shows that mothers who experience hunger or stress during their pregnancies can transmit these lived experiences through chromosomal changes to their children. This, in turn, increases their children’s risk for chronic conditions like diabetes or heart attacks as adults.
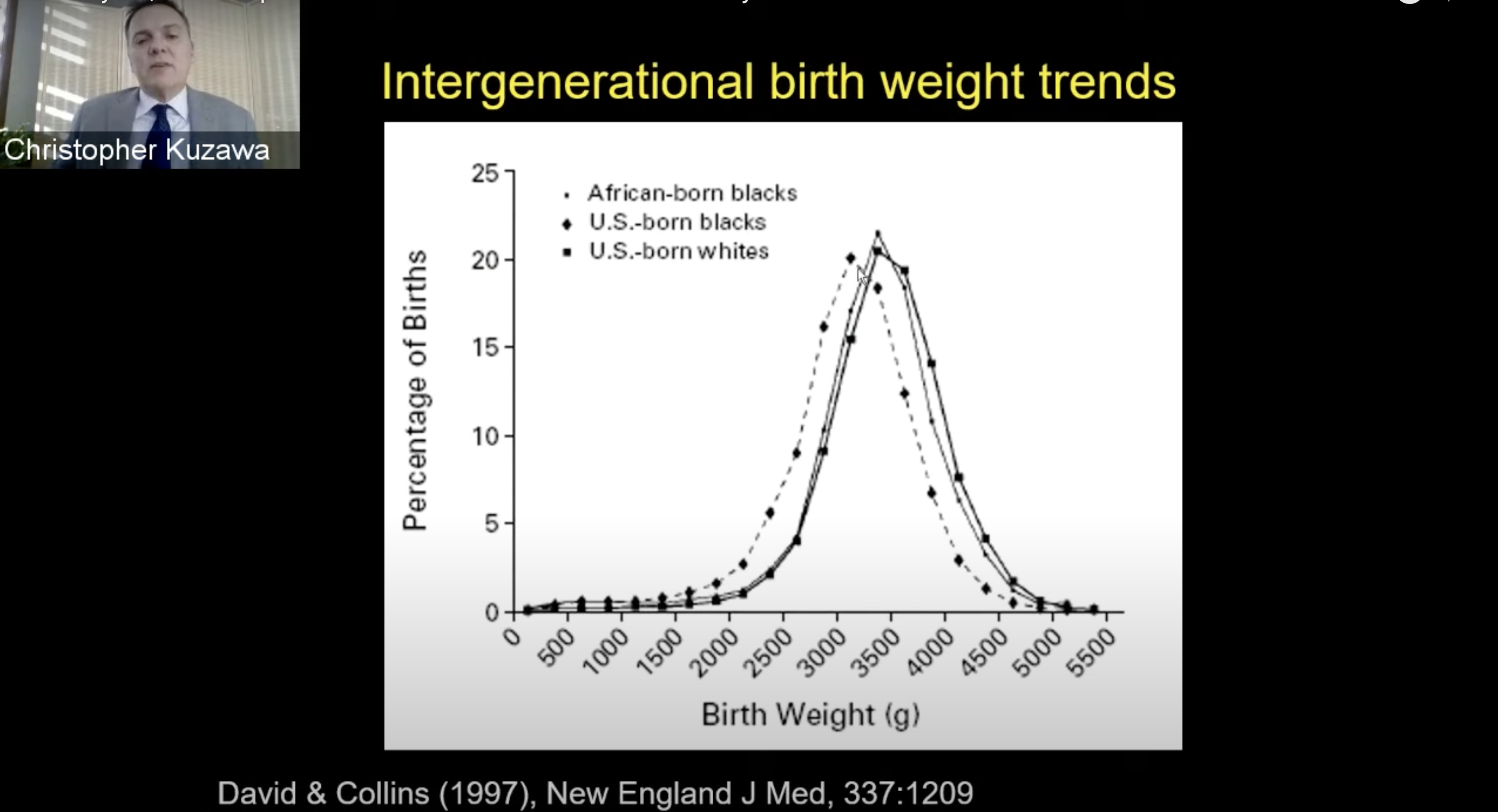
In considering how all of this plays into U.S. health disparities specifically, Kuzawa again pointed to major disparities in health between Blacks and Whites. He referred to a study of Black African immigrants to the U.S. that showed that their birth weights were initially similar to those of Whites. Once the immigrants settled in the U.S. and started having children, however, birth weights in future generations went down.
“There’s something about being Black in America that’s driving birth weights down,” he said. “It’s not a genetic factor.”
He also cited another study finding that mothers with distinctive Arab names had smaller weight babies, following the 9/11 attacks in 2001. It underscores the role of systemic racism.
Overall, Kuzawa notes that the evidence underscores how both positive and negative stressors—like coping and social capital on the one hand and stress and racism on the other—influence a mother’s biology, which in turn, affects short-term birth outcomes like birth weight and fetal development.
“But unfortunately, the story does not end there,” he said.
“There’s good evidence that some of these early-life factors are going to set up risk for some of these late life factors,” he continued, noting the effects on later generations.
In summary, he noted how African Americans have, on average, lower birth weights that are due to social causes, not genetic factors, and lower birth weights can lead to cardiovascular and other chronic diseases in adults.
For Kuzawa, the evidence from his and others’ research on developmental origins is clear: Improved economic, housing, or education opportunities for Black Americans can reverse these inequities and narrow the racial gap in adult health.
“So, this is partly a story about how health inequality today traces to racial injustices in the past,” he said. “But it also shows that policy changes that improve things now are going to have benefits that reverberate into the future as well.”
Watch his complete testimony and read his op-ed.
Christopher Kuzawa is the John D. MacArthur Professor of Anthropology.
Photo credit: California Department of Justice
Published: August 3, 2023.


