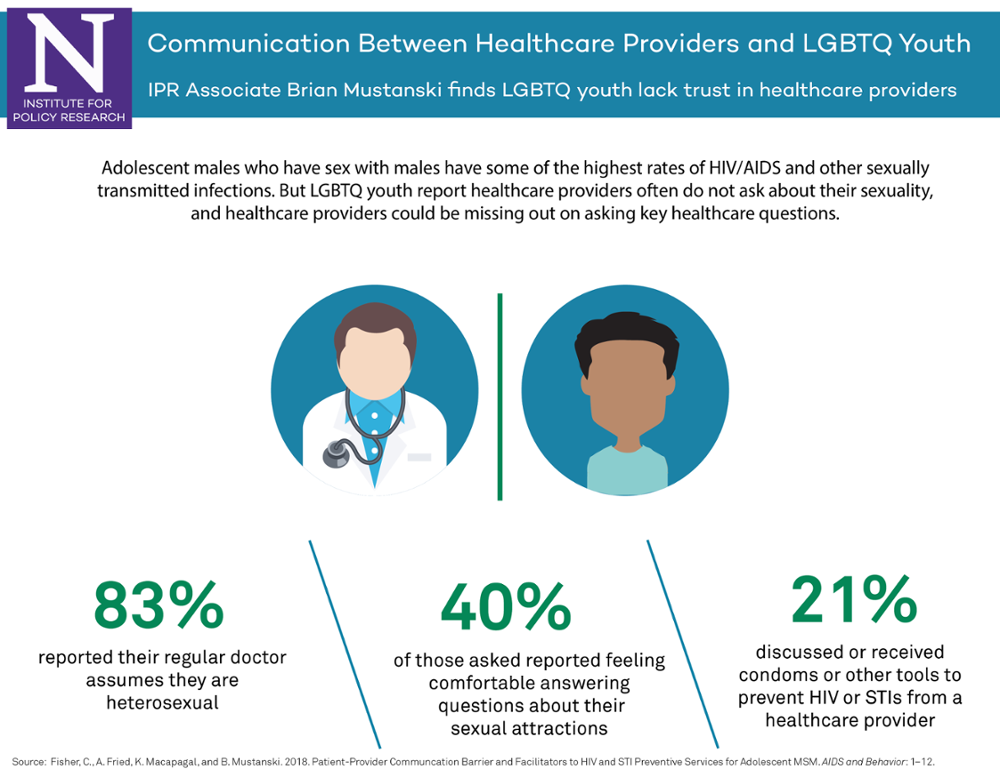
Communication Between Healthcare Providers and LGBTQ Youth
IPR associate Brian Mustanski finds LGBTQ youth lack trust in healthcare providers
Get all our news
Young men who have sex with men have some of the highest rates of new HIV infections. But LGBTQ youth’s experiences with healthcare providers could be a barrier to receiving prevention information and testing, according to a new study by IPR associate Brian Mustanski. Mustanski is a professor of medical social sciences and director of the Institute for Sexual and Gender Minority Health and Wellbeing at Northwestern University.
Click on the image above to see a larger version of the infographic.
In a survey of 198 male adolescents who have sex with males, Mustanski and his colleagues discover that healthcare providers had only asked 20 percent of them about their sexual orientation or attraction. Almost three-quarters of the young men believed their doctor just assumed they were straight. The youth also reported being more uncomfortable in discussing their sexual orientation with their doctors—more so than with their school counselors or mental health professionals.
Not discussing their sexual orientation with their doctors meant these young men might have missed receiving important information about their sexual health, Mustanski and his co-authors find. Less than half indicated they had received any prevention services for HIV or sexually transmitted infections (STIs) from their doctor. Study participants were significantly more likely to receive HIV and STI prevention information and services within the past year if their doctor had asked them about their sexual orientation.
Given the demands of medical professionals, the researchers note in AIDS and Behavior that doctors typically cannot afford to wait for young patients to raise the subject of their sexual orientation. Young men who have sex with men have some of the highest rates of new HIV diagnoses, and they are more likely than their straight peers to engage in risky sexual behaviors such as having sex without a condom.
Why were so many of these young men hesitant to broach the topic of their sexual orientation? Many reported being worried that their healthcare provider would out or stigmatize them. Though most did not directly experience discrimination against gay men in medical settings, more than half believed that LGBTQ patients do not receive equal treatment.
The survey results highlight the importance of patient trust in sexual healthcare. Mustanski and his colleagues suggest that enhanced LGBTQ training for pediatricians and primary care physicians can help create more open patient-provider communication and lead to more positive early healthcare experiences.
Brian Mustanski is professor of medical social sciences, director of the Institute for Sexual and Gender Minority Health and Wellbeing, and an IPR associate.
Published: May 18, 2018.